Services
Cataract Surgery
A cataract is simply an opacity, or cloudiness in the lens. Cataracts can be tiny spots, patchy or linear areas, or can occupy the entire lens. A complete ocular exam involving all structures of the eye is required to fully evaluate the cataract and the prognosis for surgery. If there is significant vision loss and the cataract has not progressed to cause other issues inside the eye, then surgery to remove it is possible. For good candidates, the success rate is 90-95%.
Surgery performed on cataracts that have not been present for an extended time carries a better prognosis with a decreased chance of post-operative complications. Surgery may be recommended in one or both eyes. Prior to surgery an electroretinogram (ERG) and ocular ultrasound will be performed to evaluate your pet’s retinal function. Your pet’s risk of glaucoma may be evaluated via gonioscopy prior to surgery as well.
Early evaluation of cataracts is optimal for your pet’s ocular health, even if surgery is not an option. Painful complications can sometimes arise inside the eye if the cataracts are not removed. Many of these complications can be prevented with an early evaluation and medications.



Corneal Ulcers: Medical and Surgical Treatments
Ulcers/Lacerations: The cornea is the clear outer surface of the eye. Corneal ulcerations occur when the outer-most layer of the cornea (the epithelium) is damaged. The ulcer or laceration can remain superficial or it can involve the deeper layers of the cornea. Some ulcers can become rapidly infected necessitating aggressive topical antibiotic therapy. Superficial ulcers usually heal quickly with little to no scarring. In comparison, deep ulcers or lacerations may require surgery to “patch the defect”. This emergency surgery is known as a conjunctival graft.
A Descemetocele is a condition in which the inner-most clear layer of the cornea becomes visible. When this occurs, it is considered a surgical emergency since the eye is at a very high risk of rupture. Another serious surgical emergency is considered a full thickness globe perforation or full thickness laceration. If the underlying cause is not corrected, then ulcer may recur or worsen.
Glaucoma Diagnosis, Treatment and Surgery
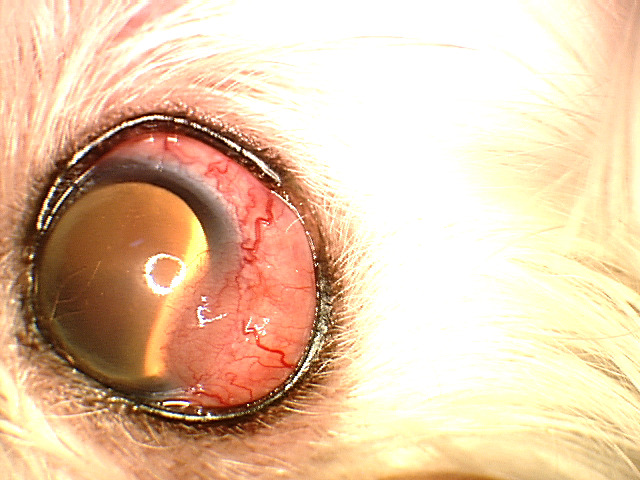
Glaucoma is a collection of diseases where the pressure in the eye is too high, causing permanent damage to the optic nerve and the retina as well as pain. The diagnosis of glaucoma is based on history, clinical signs, tonometry (eye pressure measurement), and sometimes gonioscopy. Gonioscopy is a technique useful in determining the nature of the glaucoma (inherited versus secondary) and will provide insight as to whether the unaffected eye is at risk. Redness of the conjunctiva (white part of the eye), clouding of the cornea, dilation of the pupil, and pain are common clinical signs of glaucoma. In the later stages, the eye may become enlarged.
Determining the type of glaucoma is critical in our ability to treat it. Dr. Sigle has received advanced training in differentiating and treating the many forms of glaucoma. Treatment recommendations may involve medications, surgery, or both. Glaucoma in animals can rapidly progress to permanent blindness in a very short time if not diagnosed and treated. Early intervention is key in our ability to preserve vision and prevent and/or treat pain.




Eyelid Masses
Eyelid masses are most often benign in the dog. Cats have a higher incidence of malignant eyelid masses. Depending on the size, location, and appearance of the mass your doctor may recommend taking a sample of the mass (biopsy or fine needle aspirate) to determine the mass type prior to definitive surgery.
Small masses can often be removed by debulking the mass, curetting out any clogged secretions from the underlying glands, and freezing (cryosurgery) of the underlying tissue.
Small masses extending into the eyelid tissue will require a more invasive procedure called a wedge resection. We may recommend submitting the mass for histopathology in these cases.
If the mass involves more than one third of the eyelid margin, surgical reconstruction (blepharoplasty) of the eyelid is usually necessary. This may require more complicated procedures that mobilize the surrounding skin to recreate a new eyelid margin.
Even benign eyelid masses can lead to corneal irritation and ulcers, eye and eyelid infections, corneal scarring, corneal vascularization, and corneal mineralization. Some of these complications can be painful and cause vision loss.
Dry Eye Disease
Keratoconjunctivitis sicca (KCS) or Dry Eye results from lack of aqueous tearing. This drying can lead to corneal ulcers, corneal rupture, ocular infections, significant patient discomfort, corneal scarring, corneal vascularization, and corneal mineralization. The most common cause of KCS in animals is due to an immune-mediated inflammation of the lacrimal and third eyelid glands. Other causes of KCS include: neurogenic, congenital, traumatic, or iatrogenic (removal of a prolapsed third eyelid gland).
Diagnosis is based on history, clinical signs and a number of diagnostic procedures. These include the Schirmer Tear Testing (STT) which measures watery tear production. Fluorescein stain (a bright green stain) is used to define breaks in the corneal surface and the rate of tear film breakup. Most cases of KCS can be managed medically, although cases that do not respond to medications can be treated with a surgery called a Parotid Duct Transposition.
If medical management is successful, treatment will need to be life-long.



Inflammatory Diseases of the Eye
Inflammation is a non-specific condition where tissues are red, swollen, sore and the blood
vessels are dilated and leaky, causing edema. This can happen in any tissue of the eye of
adjacent structures. In medical terminology “itis” means inflammation.
- Blepharitis: Blepharitis is an inflammation of the eyelids. It may also refer to an
inflammation of the tiny glands of the eyelid margin called the meibomian glands. - Conjunctivitis: The conjunctiva is the pink tissue that lines the inner surface of the
eyelids and covers the white portion of the eyeball (sclera). It is a protective layer that
contains special glands that secrete a component of the tear film that helps maintain
normal eye health. Conjunctivitis is a condition where the conjunctiva becomes
reddened, congested, and painful. - Episcleritis: Episcleritis usually appears as an immovable pink lump or nodule on the
white part of the eye. It may also be more generalized and appear as redness and
apparent swelling of the eyeball. With severe reactions, small blood vessels may grow
into the cornea and cause it to become cloudy. - Keratitis: Keratitis is inflammation in the cornea. Common clinical signs include
pigmentation (brown discoloration), vascularization (blood vessel in-growth) and
opacification (haziness) of the cornea. These corneal changes may lead to scarring and
may progress to severe visual impairment or blindness in severe cases. - Uveitis: Uveitis is an inflammatory process involving the iris and the choroid (vascular
layer) in the back of the eye. Uveitis results in the fluid in the eye becoming cloudy. The
debris produced by uveitis can block the drainage angle and result in increased
intraocular pressure (glaucoma) over time.
Determining the underlying cause of the inflammation is paramount to effective treatment.
Retinal
Retinal and Optic Nerve Disease

What is the retina? The retina is a delicate tissue situated in the back inside wall of the eye. It serves as a screen on which incoming light is focused through the cornea and lens. It has two primary photoreceptor cells; rods and cones. Once light strikes these retinal cells, the light impulse is changed into a signal which is interpreted by the brain as vision. The signal is sent to the brain via the optic nerve.
- Retinal Degenerations may be inherited (Progressive Retinal Atrophy), due to old age, or secondary to an external cause including: drug toxicities, old age, infection, inflammation, radiation therapy, nutritional deficiencies, end-stage glaucoma and idiopathic causes. Retinal degeneration in small animals primarily affects the photoceptors (rods and cones) causing the retina to become thinner and lose function. In most cases there is no treatment that will restore vision.
- Sudden Acquired Retinal Degeneration (SARD): Sudden Acquired Retinal Degeneration (SARDs) is characterized by acute vision loss, usually over a 1-5 day period. Initially the retina appears normal so diagnosis by performing a test of retinal function, called an ERG (electroretinogram) is necessary to differentiate it from a disorder in the brain. There is currently no successful established treatment for SARDs.
- Hypertensive Retinopathy: High blood pressure can cause damage to the small blood vessels in the eye. When this occurs, the vessels become leaky and allow fluid to accumulate underneath the retina, causing it to elevate and detach. High blood pressure is often the result of a systemic disease. Heart disease and kidney problems are the most common. The diagnosis is based on clinical signs and measuring blood pressure. The prognosis for retinal reattachment is dependent on the extent of the damage and if there is any associated bleeding. In some cases, if diagnosed early, retinal reattachment can occur, and vision can be restored to some extent.
- Retinal Detachment (Tears): A detachment of this type is where a portion or the entire retina “peels off” the back wall of the eye. Common causes for detachment include: inherited retinal defects, advanced cataracts, high blood pressure, inflammation and trauma. Vision loss is directly related to the amount of the retina that is detached. In very few cases the retina can be reattached surgically.
OFA CAER exams
The purpose of the OFA Companion Animal Eye Registry (CAER) is to provide breeders with information regarding canine eye diseases so that they may make informed breeding decisions in an effort to produce healthier dogs. CAER certifications will be performed by board certified (ACVO) veterinary ophthalmologists. Regardless of whether owners submit their CAER exam forms to the OFA for “certification,” all CAER exam data is collected for aggregate statistical purposes to provide information on trends in eye disease and breed susceptibility. Clinicians and students of ophthalmology as well as interested breed clubs, individual breeders and owners of specific breeds will find this useful.
In the interest of creating a faster and more stream-lined process, OFA has created an on-line form you should create prior to your appointment with us. Please see the following information about creating your form online through their website: www.ofa.org.
To register your pet for a CAER Exam:
- Go to www.ofa.org
- Create an account or Log In to your existing account
- Go to Create a New Application
- Follow the OFA Online Road Map
- In the Exam/Service Section, select Online Veterinary Exam
- Select In a Veterinary Office
- Search by last name only. Enter Sigle in this section
- When complete, you will receive an email from OFA confirming that your application has been created.
There is a $15 fee to register but your card will not be charged until the application is processed.
For additional information, you can contact OFA at 573.442.0418 or email at [email protected].
